03
07/2022
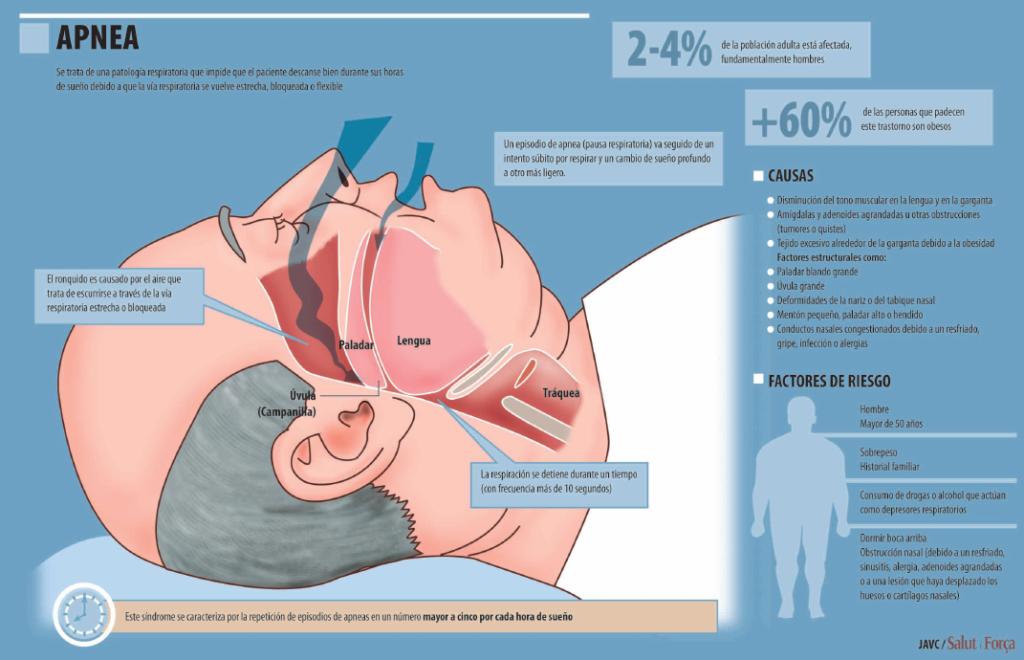
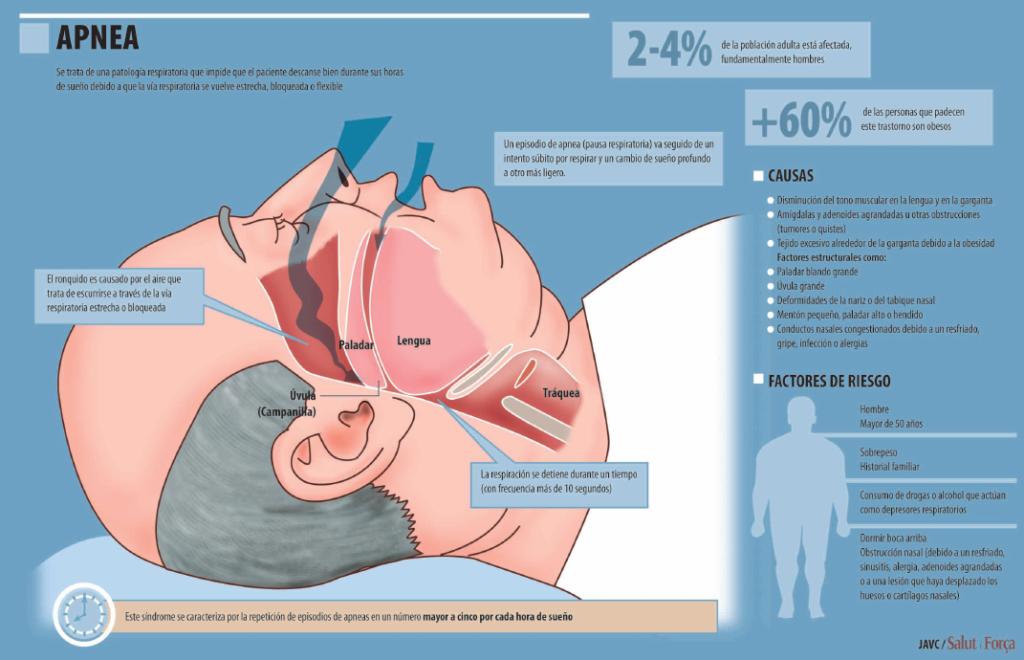
Sleep apnea is manifested by micro-awakenings as a result of the sleeper having lost their breath, although the patient does not perceive it and believes that they have slept all night / Interruption of the sleep cycle causes severe daytime sleepiness and can lead to complications or risk of heart disease with episodes that can end in death
Do you have sleep apnea? Probably in its initial stages you will be the last to find out, or even if you begin to suspect that something is wrong with you, that you are not sleeping well although you apparently sleep enough and all at once, it will not occur to you that the origin of the problem is that at night you he is left without breathing and drowning wakes him up for a few moments.
An awakening that lasts very little, so little that the sleeper does not regain consciousness, but the sleep cycle is interrupted and begins again, so that even if the eight hours are spent in bed and even if they don't wake up, remember having been awake, the person has not slept well, what's more, they are sleepy all day, they even fall asleep anywhere.
People who suffer these micro drownings and micro awakenings incur several risks if the problem is not treated. The first, as has already been said, derived from not having slept well: they fall asleep anywhere: tying their shoes, eating... or driving.
Serious accidents involving people who fall asleep while driving usually have that cause as their origin. But the problem is not only to fall asleep anywhere, to be sleepy all day.
People with sleep apnea are part of the risk group of those who can develop serious cardiovascular diseases. The good news is that apnea, if diagnosed and treated early, can be cured. But you must not let time pass.
HAVE YOU HEARD ABOUT SAHS?
Sleep apnea-hypopnea syndrome (SAHS) is the most common respiratory disorder that occurs during sleep, affecting around 4% of adults, according to epidemiologists. It has also been called syndrome of hypersomnia and periodic breathing (SHRP), and Pickwick syndrome associated with obesity.
It is currently called Obstructive Sleep Apnea Syndrome (OSAS, in Anglo-Saxon literature), Obstructive Sleep Apnea Syndrome (OSA) or simply Sleep Apnea Syndrome (SAS), which included all other diseases derived from this type of disorder. The use of the term SAHS is recommended.
As experts explain, sleep apnea is a common disorder in which a person has one or more pauses in breathing or has shallow breaths during sleep. Pauses can last from a few seconds to several minutes. They usually occur 30 times or more per hour. Breathing returns to normal and the patient is usually unaware of anything.
Those who sleep next to those who suffer from this problem tend to detect both micro-awakenings, in which the person seems to be drowning, running out of breath -as is actually the case- to returns to normality, that in Sometimes they occur with a loud snore or with a sound similar to what a person makes when choking.
UNDERDIAGNOSTIC
Specialists point out that sleep apnea often goes undiagnosed because the family doctor does not find it normal or through an analysis: the family doctor must suspect that something is wrong -when taking the medical history- and refer the case to special units of hospital pulmonology services.
The most common type of sleep apnea is obstructive sleep apnea, a condition in which the airways become narrowed or blocked while you sleep. When the sleeper tries to breathe, the air that manages to pass through the obstructed part can cause loud snoring. Obstructive sleep apnea is more common in people who are overweight.
However, it can also affect anyone. For example, young children with swollen tonsils may have obstructive sleep apnea. Central sleep apnea is a less common type and occurs when the part of the brain that controls breathing does not send the correct signals to the respiratory muscles.
As a result of this dysfunction, the patient does not make efforts to breathe at certain times, for short periods. Central sleep apnea can occur in anyone. However, it is more common in those who suffer from certain diseases or use certain medicines. Snoring usually does not occur in central sleep apnea.
C0MPLICATIONS
Going back to apnea as a general disease, specialists point out that if this pathology is not treated it can increase the risk of high blood pressure, heart attack, cerebrovascular accident (stroke), obesity and diabetes. Also, increase the risk of external heart failure occurring.
Another of its possible complications is increasing the chances of having arrhythmias or irregular heartbeats, as well as the chances of suffering car or work accidents (by falling asleep in risky circumstances without being able to avoid it). Sleep apnea is a chronic health problem that requires long-term treatment.
The Diagnosis of Sleep Apnea-Hypopnea Syndrome requires a sleep study called polysomnography or polygraphy, without which it is not possible to confirm the pathology. The polysomnographic study includes three basic studies: electroencephalography (EEG), electrooculography (EOG), and electromyography (EMG).
Other parameters analyzed in the diagnostic process of this type of patient are electrocardiography, pulse oximetry, respiratory effort, transcutaneous CO2, a recording of sounds to evaluate snoring, performing an EMG test of the extremities and continuous video monitoring of the patient during a night's sleep.
POLYSOMNOGRAPHY
Polysomnography (PSGN) is a test that is done overnight. Experts comment that despite being full of sensors -in the case of suspected sleep apnea- and knowing that they are being monitored, they do not take long to fall asleep, such is the fatigue and sleepiness accumulated by patients who 'believe' that They sleep, but they don't.
This test involves placing sensors at key points on the head and chest to record brain activity, breathing, heart rate, muscle activity, and blood oxygen levels while falls asleep, all of which varies significantly if you have sleep apnea (and other conditions).
Before the test begins, the patient is prepared for the study, placing electrodes (sensors) on the scalp and other parts of the face and body, as well as different sensors to assess cardiorespiratory function. Despite this, apnea sufferers fall asleep almost instantly, as noted above.
The test lasts for about 8 to 9 hours, that is, the night of sleep of a normal person, although the preparation that is necessary means that the patient must be there a little before sleeping and leave a little after waking up. After performing the test, you can immediately return to normal activity, or as normal as any other day.
TEST WITHOUT PROBLEMS
Regarding the preparation, it is advised that the usual medication can be taken, with the exception of drugs that may affect sleep. About these medicines it is advisable to consult the doctor. It is a diagnostic, non-therapeutic test, whose risks are usually minimal, but rather non-existent due to the smoothness and simplicity of the process itself.
Only in patients with sensitive skin, the necessary scraping of the skin to remove hair, necessary for the placement of the sensor electrodes, can cause small irritations, which improve spontaneously over time and without causing any further problems. of this or another kind. It is a painless and discomfort-free test PSGN is performed on patients suspected of having sleep amneas (or other sleep disorders) of any age and in any situation.
How to use Search Google...like a pro. Me too, just got to know it. Good info. 🙂👍👍Source from LearnComputer https://t.co/NzFTxIqyvA
— azmiie YAMA 🎵🎶™️ 🇵🇸🤝🇲🇾 Wed Jul 21 02:24:59 +0000 2021
The only exception would be in people with a known allergy to some of the materials used for the test, although there is the possibility of replacing them with non-allergenic ones, according to the specialists.
It is possible to carry out the test at the patient's home (if they have mobility problems), with health supervision throughout the night to ensure that it is carried out correctly. However, it is normal for it to be carried out in a hospital environment, in health centers that have the appropriate facilities and the so-called Sleep Disorders Units.
ALL ABOUT SLEEP
In summary, the PSGN studies the cycles and stages of sleep, the flow of air in and out of the lungs, the levels of oxygen in the blood, the position of the body, the brain waves (EEG), the effort and respiratory rate, electrical activity of muscles, eye movements, and heart rate, all affected by apneas if they occur.
Once sleep apnea is diagnosed, specialists point out, without wanting to be alarmist, that not treating it can lead to a fatal outcome.
Excessive daytime sleepiness can cause people to fall asleep at inappropriate times, such as when they are driving a car, as mentioned above.
But it also appears that sleep apnea also leads to an increased risk of strokes and transient ischemic attacks (also known as "mini-strokes"), and is associated with coronary heart disease, heart failure , irregular heartbeats, heart attacks and high blood pressure.
Although there is no proper cure for sleep apnea, recent studies indicate that successful treatment can reduce the risk of heart and blood pressure problems. There are currently several treatments for sleep apnea, depending on the medical history and severity. Almost all treatment regimens begin with lifestyle changes.
HEALTHY LIVING
Again, the doctor will advise avoiding alcohol and medications that relax the central nervous system (sedatives and muscle relaxants), losing weight (if there is excess, which is common in these patients) and quitting smoking.
Some people get better with special pillows or devices that keep them from sleeping on their backs. Oral appliances are also used to keep the airway open during sleep.
This is a mask that is placed with a design that guarantees comfort and does not impede sleep and that, by means of positive air pressure in the patient's airways, maintains breathing adequately throughout the night and prevents the apneas.
It is when conservative methods –healthy lifestyles among them– are insufficient when that continuous positive airway pressure (CPAP) device is prescribed, which consists of connecting a face mask to a tube and a machine that blows pressurized air into the mask and through the airway to keep it open.
There are also surgical procedures that can be used to remove tissue and widen the airway. Some people may need a combination of therapies to successfully treat their sleep apnea. The specialized doctor will indicate the seriousness and/or complexity of the case and will determine the treatment or combination of therapies that must be carried out.
URINE AT NIGHT
Among the side effects of sleep apnea there is one that is not so serious but that does mean a loss of quality of life for those affected. According to a recent article by Robert Preidt published in HealthDay, managing sleep apnea could reduce the number of times certain patients interrupt their sleep each night to get up to urinate.
“A US expert who reviewed the new findings said sleep apnea and overactive bladder at night often go hand in hand. No one knows for sure why this association occurs, although there are plausible theories, said Dr. Alan Mensch, chief of pulmonary medicine at Plainview Hospital in Plainview, New York.
He adds: “Untreated sleep apnea patients produce a greater volume of urine at night, Mensh noted. In addition, the decrease in oxygen that occurs in sleep apnea episodes stimulates blood flow to the kidneys, and simply waking up could also make people more aware of the need to urinate." To treat this problem and others related to sleep, scientific associations of great specific weight such as the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) value the development of sleep units in hospitals. This is explained in an article published in Archivos de Bronconeumología.
SLEEP UNITS
In the article signed by the specialists Nicolás González Mangado, Carlos Egea Santaolalla, Eusebi Chiner Vives, Alberto Capelastegui Saiz and Pilar de Lucas Ramos, the sleep unit is defined as an interdisciplinary entity, made up of specialized personnel and medical teams to diagnose and treat sleep disorders, monitoring and control.
According to this article, among the 741 centers contacted in Spain, 217 regularly evaluated patients with SAHS.
88% had respiratory polygraphy or polysomnography.
The average delay in consultation was 61 days, and the average delay for PR was 224 days.
The mean of PR teams was 0.99/100,000 inhabitants, when the recommended rate is 3/100,000.
SEPAR promoted the accreditation of sleep units, whose main objective was to ensure and improve the care of our patients. So far (a few years ago from the study) 31 had been accredited as multidisciplinary and another 35 as respiratory units. A new guide for the accreditation of sleep units has recently been promoted.
The article explains that the SEPAR Sleep Area has led the accreditation of sleep units in Spain.
Most are run by pulmonologists, covering an organizational spectrum, from sleep units with the capacity to solve most problems related to sleep disorders, to purely respiratory units.
COMPLETE CARE
Its objectives are to improve the level of care for patients, ensuring a framework of quality care; establish resources and facilitate their management; promote the development of training plans in sleep disorders and advance the concept of accreditation of knowledge; encourage collaboration with professionals from other clinical disciplines.
A sleep unit is a network (basic concept) in which different healthcare links intervene, from family medicine to extra-hospital specialists and referral and non-referral centers.
The goal of pulmonologists should be to evaluate and direct the so-called sleep care network. For this, a model should be implemented.
This model should include, according to the SEPAR specialists, a sleep center, sleep schools, expert primary care physician, tutor patient..., assuming evolutionary control, supported by expert nursing and telematic incorporations, all under the leadership of the dream unit, as reflected in the aforementioned article.
- 833
- can you get facial hair with a cpap mask
Related Articles
How to remove blackheads from the nose - Tips and tricks
04/02/2022Rating: 4.6 (20 votes)3 commentsBy Marta Vicente. Updated: September 10, 2021 Blackheads are very common in some areas of the face, such as the nose, since it is in these places where...
5 tourism innovations born in the pandemic that have come to stay
01/02/2022In the 20 months since the start of the COVID-19 pandemic, technological innovations have gone from futuristic to familiar. Nowadays it has become habitual in our day to day...
Get all the information you need for Miami Ultra Music Festival 2018 Get all the information you need for Miami Ultra Music Festival 2018
31/01/2022Are you ready for Ultra Miami next week? If so, it doesn't hurt to maximize your experience with this essential information.Ultra Music Festival is preparing to open its doors next...
47 Best Mustache Stain Cream in 2022 [Based on 642 Reviews]
25/02/2022Rosario Jaramillo The key to buying the right mustache stain cream is to make sure the one you're buying meets all of your needs. However, with so many options available...